Services: Ear, Nose & Throat
Sleep apnea is becoming increasingly common in the American population. Adequate sleep is an absolute necessity for normal human function. Most experts believe the average adult requires 7 to 8 hours of normal sleep for good health and optimal performance. Sleep restriction or interruption of 6 hours or less has been shown to cause cognitive performance deficits and fatigue. The Southeastern ENT, Allergy, & Sleep Disorders Institute is dedicated to treating the entire spectrum of sleep conditions which may impair a normal quality of life.
Sinus Surgery
Ear Tubes
Eardrum Repair
Adenoidectomy
Deviated Septum Repair
Nasal Obstruction Surgery
Sleep Apnea Treatment
Botox® & Fillers
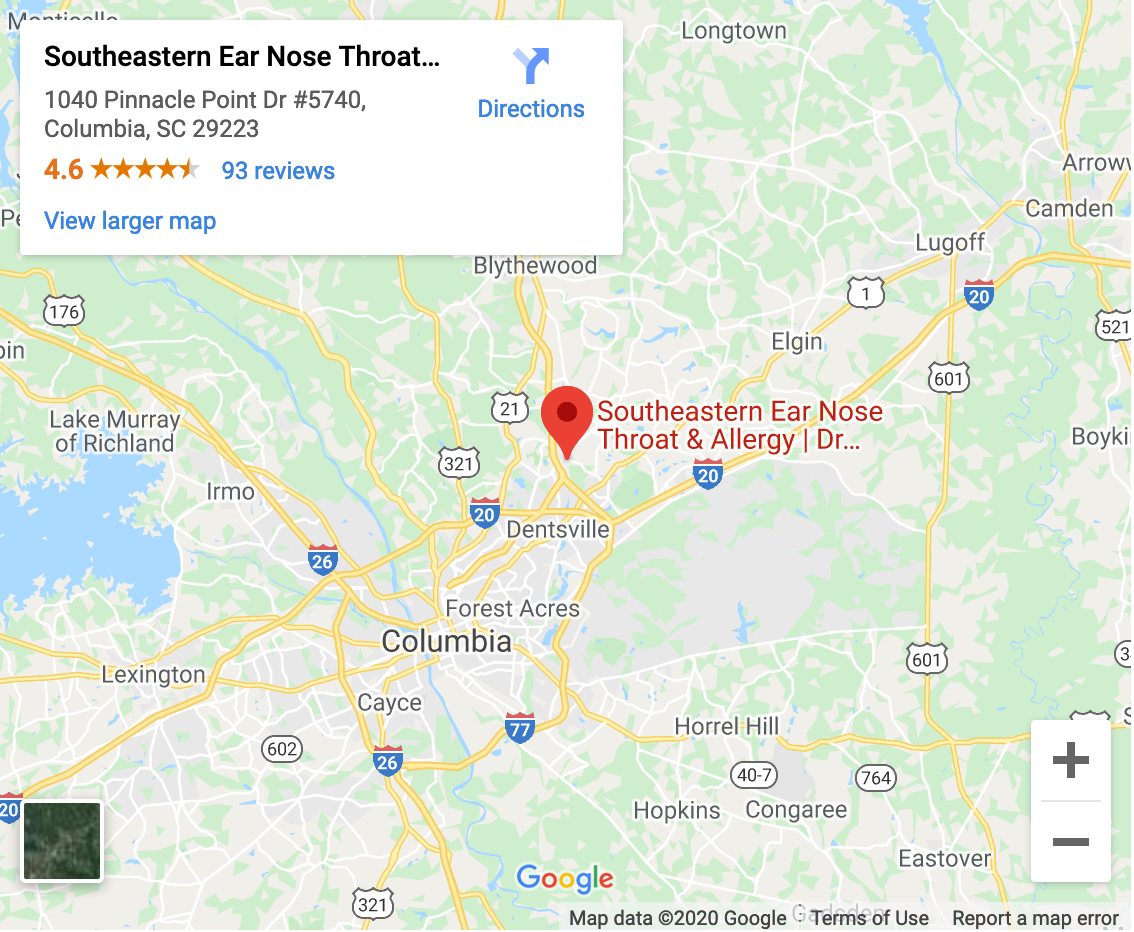
Office Hours
| Mon - Thur | 8:00 - 5:00 |
| Fri | 8:00 - 4:00 |
Allergy Shot Hours
| Mo, Tu, Th | 8:10 - 4:45 |
| Wed | 1:00 - 4:45 |
| Fri | 8:10 - 3:45 |
Make An Appointment
We look forward to caring for you!
(803) 509-7200
Visit Our Office
Detailed Descriptions
Functional Endoscopic Sinus Surgery (FESS)
Standard Sinus Surgery
Endoscopic sinus surgery uses small nasal endoscopes to open the natural pathways that drain the sinuses. It is used to treat patients who have chronic sinus issues. The nose and sinuses are part of the upper respiratory tract system. The function of the nose is to warm, humidify, and filter the air that passes through it. The true function of the sinuses continues to be debated, but it is imperative that the sinuses remain patent and drain normally. If the sinuses become blocked, normal sinus drainage is hindered and sinusitis can develop. Patients with chronic sinusitis have significant impairment in their quality of life.
What Are Sinuses?
There are four paired sets of sinuses in the facial skeleton: 1) the Maxillary sinuses are located beneath the cheeks right under the eyes, 2) the Frontal sinuses are situated behind the forehead above the eyes, 3) the honeycomb shaped Ethmoid sinuses are set between the eyes, and 4) the Sphenoid sinuses are located deep in the nose and below the brain. Each of these is enclosed in a space that drains through an opening (ostium) into the nose. These ostia can become blocked due to inflammation/swelling of the mucosa lining or by tumors or bony structures (turbinates).
Effects of Blocked Sinuses
The term sinusitis refers to inflammation of the sinuses. Common causes of inflammation in the nose are allergies (“hay fever”), acute viral infections, or tobacco smoke. Other important causes include bacterial infections, fungal/mold allergies, and obstructive inflammation due to polyps or abnormally enlarged turbinates. There are two major types of sinusitis:
- Acute sinusitis is an infection that resolves in less than four weeks.
- Chronic sinusitis involves recurring or persistent infections and symptoms that can last twelve weeks or more. Complications from sinusitis include infections that can spread to the eye socket (orbit) creating a risk for loss of vision or blindness or spread to the brain resulting in meningitis or a brain abscess.
Most Common Symptoms of Blocked Sinuses/Sinusitis
- Recurring sinus infections
- Thick yellow or green nasal discharge
- Persistent nasal drainage and congestion
- Upper tooth pain
- Frontal headaches and/or facial pressure
- Fever, fatigue and malaise
Treatments for Blocked Sinuses
Our physicians may treat acute or chronic sinusitis with antibiotics, decongestants, nasal steroid sprays, antihistamines and/or flushing of the sinuses. As practicing allergists and Member and Fellow of the American Academy of Otolaryngic Allergy, our physicians also evaluate the possible role of environmental allergies causing the sinus symptoms and treats these appropriately. If these medical treatments fail, surgery may be required to enlarge the sinus openings in order to restore normal sinus function and breathing. Functional Endoscopic Sinus Surgery employs state-of-the-art technology and is one of today’s safe and effective ways to restore normal sinus function and breathing. It is performed through the nose using small telescopes and requires no external incisions. Our physicians have extensive experience with Functional Endoscopic Sinus Surgery and decide upon a treatment plan for each individual patient.
Balloon Sinuplasty
Minimally Invasive Sinus Surgery
Balloon Sinuplasty employs small nasal endoscopes and dilating balloons to safely and effectively widen specific sinus openings. The nose and sinuses are part of the upper respiratory tract system. The function of the nose is to warm, humidify, and filter the air that passes through it. The true function of the sinuses continues to be debated, but it is imperative that the sinuses remain patent and drain normally. If the sinuses become blocked, normal sinus drainage is hindered and sinusitis can develop. Patients with chronic sinusitis have significant impairment in their quality of life.
What is Balloon Sinuplasty?
Balloon Sinuplasty is an FDA approved procedure that safely and effectively widens the sinus openings, without trauma to surrounding tissues, while preserving the natural sinus openings. Balloon Sinuplasty is a technique similar to Angioplasty that uses balloons to dilate the sinus openings instead of using microdebriders and forceps. While it is less traumatic than traditional sinus surgery (FESS), it is NOT indicated for every patient with sinus symptoms and must be tailored to each individual patient.
What Are Sinuses?
There are four paired sets of sinuses in the facial skeleton: 1) the Maxillary sinuses are located beneath the cheeks right under the eyes, 2) the Frontal sinuses are situated behind the forehead above the eyes, 3) the honeycomb shaped Ethmoid sinuses are set between the eyes, and 4) the Sphenoid sinuses are located deep in the nose and below the brain. Each of these is enclosed in a space that drains through an opening (ostium) into the nose. These ostia can become blocked due to inflammation/swelling of the mucosa lining or by tumors or bony structures (turbinates).
Effects of Blocked Sinuses
The term sinusitis refers to inflammation of the sinuses. Common causes of inflammation in the nose are allergies (“hay fever”), acute viral infections, or tobacco smoke. Other important causes include bacterial infections, fungal/mold allergies, and obstructive inflammation due to polyps or abnormally enlarged turbinates. There are two major types of sinusitis:
- Acute sinusitis is an infection that resolves in less than four weeks.
- Chronic sinusitis involves recurring or persistent infections and symptoms that can last twelve weeks or more. Complications from sinusitis include infections that can spread to the eye socket (orbit) creating a risk for loss of vision or blindness or spread to the brain resulting in meningitis or a brain abscess.
Most Common Symptoms of Blocked Sinuses/Sinusitis
- Recurring sinus infections
- Thick yellow or green nasal discharge
- Persistent nasal drainage and congestion
- Upper tooth pain
- Frontal headaches and/or facial pressure
- Fever, fatigue and malaise
Treatments for Blocked Sinuses
Our physicians may treat acute or chronic sinusitis with antibiotics, decongestants, nasal steroid sprays, antihistamines and/or flushing of the sinuses. As a practicing allergists as well as Member and Fellow of the American Academy of Otolaryngic Allergy, our physicians also evaluate the possible role of environmental allergies causing the sinus symptoms and treats these appropriately. If these medical treatments fail, surgery may be required to enlarge the sinus openings in order to restore normal sinus function and breathing. Balloon Sinuplasty employs state-of-the-art technology and is one of today’s safe and effective ways to restore normal sinus function and breathing. It is performed through the nose using small telescopes and specialized equipment and requires no incisions. Balloon Sinuplasty cannot be used when certain anatomic obstructions exist, such as nasal polyps, tumors, or enlarged turbinates. Our physicians have extensive experience with Balloon Sinuplasty and decide upon a treatment plan for each individual patient.
Septoplasty
Deviated Nasal Septum Repair
Septoplasty is a surgical procedure used to correct defects or deformities of the Nasal Septum…often by alteration or partial removal of obstructing structures.
Statistics estimate that over 80% of all nasal septums are off-center, but this often goes unnoticed. If the septum is severely deviated away from the midline where it should be, this condition can cause problems such as breathing difficulties, nasal congestion, and perceived sinus infections. Septoplasty is a very common surgery that corrects a deviated septum and improves nasal airflow.
What is the Nasal Septum?
There is a wall inside the nose that divides the nasal cavity into halves. This wall is called the “nasal septum” and is ideally positioned precisely in the midline, thus separating the left and right sides of the nose into passageways of approximately equal size. The septum is composed of a central supporting cartilage covered on each side with mucous membrane. In many individuals, there are minor deviations of the septum due to injury sustained during childbirth and natural skeletal growth. In some individuals, due to trauma or excessive skeletal growth, the septum becomes excessively deviated and nasal obstruction occurs.
Effects of a Deviated Nasal Septum?
When the septum is significantly protruding off the midline (deviated), patients often have complaints of nasal obstruction, nasal congestion, chronic sinusitis, and headaches. A crooked septum impairs the natural flow of air through the nasal passages and can significantly affect breathing through the nose and potentially interfere with normal sinus drainage. Many patients who complain of constant sinus infections and pressure are simply suffering from impaired nasal airflow and congestion due to a deviated nasal septum. A severely deviated septum can also alter the outward appearance of the nose and can be corrected with a cosmetic surgery called Rhinoplasty.
Most Common Symptoms of Deviated Septum
- Blockage of one or both nostrils resulting in impaired daytime breathing
- Nasal congestion – may be one-sided or involve both sides
- Frequent nosebleeds
- Persistent sinus infections or facial pressure
- Facial pain, headaches, postnasal drip
- Snoring and sleep apnea
- Mouth breathing
Most Common Symptoms of Blocked Sinuses/Sinusitis
- Recurring sinus infections
- Thick yellow or green nasal discharge
- Persistent nasal drainage and congestion
- Upper tooth pain
- Frontal headaches and/or facial pressure
- Fever, fatigue and malaise
Causes of the Deviated Septum
The nose, being the most prominent figure on the face, is very susceptible to injury and a deviated septum is frequently caused by a blow to the face or it can be present at birth.
Treatments for the Deviated Septum
Septoplasty is the most common and effective treatment for a deviated septum. It is usually performed after medical therapies, such as nasal steroid sprays, are no longer effective in relieving nasal obstruction. Our physicians can determine this during your consultation. They will also determine if other causes for nasal obstruction, such as allergies or chronic sinusitis, are contributing to the underlying problem. A septoplasty is performed through the nostrils, so there is no bruising or external signs of the surgery. A turbinate reduction, whereby the internal humidifying bones of the nose are reduced in size to further improve breathing, is often performed in conjunction with a septoplasty and would be discussed prior to the procedure. A typical recovery time for a septoplasty is approximately one week.
Turbinate Reduction
Surgery for Nasal Obstruction
Turbinate reduction surgery corrects the problem of nasal obstruction by reducing the turbinate size, which decreases airway resistance, while preserving the natural function of the turbinates.
Turbinate enlargement (hypertrophy), along with a deviated nasal septum, is the major cause of nasal airway obstruction and leads to breathing problems in both adults and children.
What are Turbinates?
Turbinates are small, scroll-like bony structures inside the nose that filter and humidify air as it passes through the nostrils and into the lungs. There are three turbinates on each side of the nose: 1) inferior, 2) middle, and 3) superior. They are covered with a mucous membrane, containing vascular channels, which can swell under certain conditions such as allergies or inflammation and lead to nasal obstruction.
Effects of Turbinate Hypertrophy
An abnormally enlarged turbinate caused by inflammation typically blocks the key areas of nasal airflow and sinus ventilation. This causes nasal congestion that can mimic sinus pressure and lead to significant daytime obstruction and nighttime sleep disordered breathing. A deviated septum may also be part of the problem causing the blockage and is usually addressed at the same time as a turbinate reduction.
Common Symptoms of Turbinate Hypertrophy
- Congested or blocked nasal breathing
- Problems with night breathing
- Snoring
- Chronic sinus pressure or sinus infections
- Post-nasal drip
Treatments for Turbinate Hypertrophy
The initial treatment for enlarged turbinates is typically a topical nasal steroid or antihistamine spray. This is typically done for several weeks to evaluate if there is improvement in the nasal symptoms. Allergic rhinitis, or “hay fever,” is a common cause of turbinate hypertrophy and nasal obstruction. Our physicians include a Member and a Fellow of the American Academy of Otolaryngic Allergy (AAOA) and are certified to treat all aspects of allergic rhinitis, including adults and children who require allergy shots (immunotherapy) to control their symptoms. If medical treatment fails, then they may recommend and perform a turbinate reduction to restore the airway passages to normal size. A septoplasty is often performed in tandem with a turbinate reduction to fully correct nasal airway function.
Sleep Apnea Surgery
What is Sleep Apnea?
More than one-third of the world’s population struggles with interrupted sleep caused by lifestyle choices, work schedules, or health conditions. Sleep disorders include insomnia, persistent sleep deprivation, restless leg syndrome and obstructive sleep apnea syndrome (OSAS). These disorders usually worsen with age, but can affect both children and adults.
Obstructive sleep apnea syndrome is becoming an increasingly prevalent problem in the United States. Sleep apnea refers to a reduction or cessation of breathing during sleep and is caused by an anatomic blockage of the nose and/or throat. During sleep, there is a decrease in the activity of muscles that keep the airway patent. This leads to an increase in the collapsibility of the airway and can lead to significant airway obstruction. Patients who are overweight typically have thicker neck tissues and a smaller airway diameter that is more at risk. This obstruction greatly affects gas exchange in the lungs and can lead to lower levels of oxygen in the blood (hypoxemia). This loss of oxygen places stress on the heart and lungs and leads to “arousals” – disruptions of the normal brain activity during sleep necessary to tighten the airway muscles and restart breathing. Due to these frequent arousals, patients with sleep apnea get fragmented sleep and over time complain of nonrefreshing sleep and chronic sleepiness. Chronic snoring is a major symptom of obstructive sleep apnea and is often the reason for referral to a sleep specialist. Loud and interrupted mouth breathing is usually seen in children with sleep apnea and is often due to enlarged adenoids and tonsils.
Obstructive sleep apnea has been clinically linked with obesity, hypertension, heart and lung disease, stroke, and unexplained sudden death. It also leads to chronic daytime sleepiness that greatly impairs memory, mood, and concentration. In short, obstructive sleep apnea greatly impairs a patient’s quality of life and may pose a significant health threat.
Sleep Apnea Treatment
Non-surgical treatments for sleep apnea include lifestyle changes, oral appliances and CPAP (Continuous Positive Airway Pressure). CPAP works by applying air pressure via a mask to the nasal and oral airways to “splint” the tissues open and prevent obstruction. It is the considered the gold standard for obstructive sleep apnea treatment. When CPAP and other conservative measures fail, surgery to widen the air passages in the nose and throat is often recommended. Surgery may include the following:
- Nasal surgery to straighten the deviated nasal septum and reduce the size of the turbinates. Nasal surgery relieves the nasal obstruction component of sleep apnea and can improve CPAP compliance. Nasal surgery alone, however, rarely cures sleep apnea (less than 10%) and other interventions are usually necessary.
- Uvulopalatopharyngoplasty (UPPP) involves removing any tonsillar tissue (if present) and reducing excess length of the soft palate. It is used to relieve obstruction in the back of the throat (oropharynx). UPPP alone is not a guaranteed procedure to completely eliminate sleep apnea. In fact, a large study demonstrated that UPPP alone only cured sleep apnea in ~40% of patients. The low cure rate, however, is greatly impacted by a patient’s weight and anatomy (jaw size, tonsil size, tongue size, etc.). In properly selected patients, the cure rate with this procedure can approach 70%.
- Tongue base surgery is sometimes performed to reduce the size of an overly large or posterior displaced tongue. This enlarges the space between the tongue and the back of throat and lessens the chance of airway obstruction during sleep. As with the UPPP, patient selection and a thorough airway evaluation by an ENT specialist is critical in the decision to recommend this type of procedure.
Dr. Gunnlaugsson is certified by the American Board of Otolaryngology-Head and Neck Surgery and is also board certified in the subspecialty of Sleep Medicine. This dual Board certification involves meeting and exceeding rigorous board standards by passing exams and completing additional specialized training/education in sleep medicine. Dr. Gunnlaugsson has extensive experience in treating sleep disorders and offers the entire array of treatments for patients with obstructive sleep apnea syndrome. He can assist with lifestyle changes, oral appliance recommendations, CPAP fitting, and surgical evaluations. He performs detailed exams of the nasal and oral airways to determine where an airway obstruction may be occurring so that the proper treatment can be discussed for each individual patient.
Adenoidnectomy
Recurrent sinus and ear infections, enlarged adenoids & airway obstruction often require an Adenoidectomy…which is the surgical removal of the adenoids. Adenoids (along with tonsils) function, early in life, as the body’s first line of defense by sampling bacteria and viruses that enter the body through the mouth or nose. Over time in children, the adenoids often become diseased and enlarged to create an airway obstruction accompanied by repeated bacterial infections of the nose and ears. Removing the adenoids eliminates these problems and improves ear infections, pediatric sinus disorders, nasal obstruction, and sleep disordered breathing.
What are Adenoids?
Adenoids are a tissue mass located in the back of the nose and are similar to the lymph nodes found in the neck, groin and armpits. Unlike tonsils, adenoids are not visible through the mouth without use of special instruments. The adenoids typically shrink as we age and are often very small and insignificant in adults.
Effects Of Enlarged Adenoids (Hypertrophy)
Persistent and recurrent ear infections, breathing difficulties including snoring/sleep apnea/ loud breathing, foul breath and chronic sinus infections are common problems caused by enlarged adenoids in children and teens.
Most Common Symptoms of Enlarged Adenoids
- Mouth breathing instead of nose breathing
- “Blocked” nasal sound when speaking
- Recurring and persistent ear infections (Otitis Media)
- Snoring at night
- Breathing stops, for a few seconds, repeatedly during the night when snoring or loud breathing. This is called Sleep Apnea.
- Daytime sleepiness in adults and behavioral problems in children
- Chronic earaches/infections and hearing loss
- Pediatric sinus infections (Sinusitis)
- Persistent runny nose
Causes Of Enlarged Adenoids
Similar to tonsillitis, bacterial and viral infections in children (usually less than age 4) often cause enlargement and chronic inflammation of the adenoid pad. In some children, there is no history of infection and the adenoids enlarge due to the maturation of the immune system. The adenoids can serve as a reservoir for bacteria which are known to cause ear infections and are often removed when multiple sets of ear tubes are necessary in a child. In adults, an enlarged adenoid is rare and is often biopsied to rule out a cancerous process.
Treatments for Enlarged Adenoids
Our physicians first employ the least invasive treatment for enlarged/infected adenoids: antibiotics and observation. Surgical removal is necessary in children when breathing is hindered and sleep apnea is present. For these patients, a tonsillectomy is often performed with the adenoidectomy. Removal of the adenoid pad is also recommended when a child has persistent sinus infections which do not respond to antibiotics.
Chronic infection and enlargement of the adenoids in children can also affect the Eustachian tubes which causes recurrent, frequent ear infections and possible hearing loss. Adenoidectomy has proven to be beneficial for children with chronic ear infections and middle-ear fluid (Otitis Media), and is commonly performed in combination with Tympanostomy tube placement (Ear Tubes) in order to achieve complete relief.
Adenoidectomy is almost always done as an outpatient procedure and has a very short recovery time (usually less than 48 hours) with a minimal risk of complication.
Tympanostomy
Ventilation Ear Tubes
Tympanostomy is the placing of plastic tubes through the eardrum to allow air into the middle ear space. This is done to treat and prevent ear infections.
Otitis media refers to an infection or inflammation of the middle ear space (behind the eardrum), often preceded by a viral infection. It is a condition that occurs often in small children and less commonly in adults. Otitis media is usually caused by eustacian tube dysfunction, whereby the normal tube from the ear to the nose which opens with swallowing becomes blocked due to swelling or obstruction. This blockage prevents natural pressure equalization (“popping”) from the ear to the back of the nasal airway. This allows negative pressure to form behind the eardrum that then “pulls” in fluid from the body’s tissues. Young children (age 6 months – 2 years) are especially susceptible to otitis media as they have a shorter and more immature eustacian tube that is easily blocked. The fluid behind the ear can also become infected by bacteria, especially in children. Worsened by viral infections, a common cold and/or nasal allergies, otitis media can be very painful and can also lead to hearing loss and speech problems.
What Are Ear Tubes?
Ear tubes are tiny cylinders inserted through the eardrum (tympanic membrane) to equalize pressure in the middle ear space. Ear tubes have several names including: myringotomy tubes, ventilation tubes or PE (pressure equalization) tubes.
There are two basic types of tubes: 1) short-term and 2) long-term. Short-term tubes are smaller and typically used in children. They usually remain in place for about 6-24 months and then fall out on their own. Long-term tubes are larger and have flanges (T-tubes) to secure them within the eardrum for a longer period of time. They may fall out on their own or have to be removed by our physicians. They are often used in adults or children who have chronic ear issues or who have had several sets of short-term tubes.
Symptoms of Otitis Media
- Recurrent ear infections – viral or bacterial
- Ear pain (otalgia)
- Hearing loss
- Speech problems
Who Needs Ear Tubes?
Children and adults who suffer from repetitive or persistent middle ear infections (recurrent acute or chronic otitis media) or who have hearing loss and related speech problems secondary to ear fluid can benefit from ear tubes. Other conditions which often require tympanostomy tube placement include: 1) chronic acquired malformations of the ear drum due to chronic eustacian tube dysfunction, 2) children with Down syndrome, 3) children with cleft lip/palate, and 4) adults with chronic negative pressure, pain, and/or fluid behind their eardrums.
Positive Effects of Tympanostomy (Ventilation Ear Tubes)
- Reduced risk of future ear infections
- Restored hearing (when the hearing loss is caused by middle ear fluid)
- Improved speech
- Marked reduction in the need for oral antibiotics
- Elimination of the pain associated with negative pressure/fluid behind the eardrum
- Improved sleep in young infants
Treatments for Chronic Ear Infections
Viral ear infections typically resolve on their own while bacterial ear infections usually require antibiotic treatment. Our physicians follow this initial treatment protocol. When infections become chronic, however, tympanostomy tube surgery is often required and should always be performed by an ENT surgeon. This usually occurs when children or adults have more than 4-6 infections in a 6-12 month period or when persistent fluid is leading to chronic discomfort or hearing loss.
Tympanoplasty
Eardrum Repair
Tympanoplasty is surgery to repair/reconstruct the eardrum (tympanic membrane) usually due to a hole or perforation in the eardrum.
There are several problems that can permanently damage an eardrum (tympanic membrane) or harm the small bones (ossicles) that are located right behind the eardrum. Chronic ear infections, trauma, and prior ear tube placement can cause perforations of the eardrum while leading to hearing loss and persistent drainage of the ear that does not resolve.
What is a Tympanoplasty?
A tympanic membrane perforation is simply a hole in the eardrum. A tympanoplasty is a surgical procedure where the eardrum is reconstructed using a natural tissue graft from the patient’s body. This graft is usually tissue covering the muscle near the ear or cartilage from the ear itself. The procedure can often be done through the natural canal of the ear with a small incision behind the ear.
Symptoms of Eardrum (Tympanic Membrane) Perforation
- Persistent ear drainage
- Pain
- Hearing loss
Most Common Symptoms of Blocked Sinuses/Sinusitis
- Recurring sinus infections
- Thick yellow or green nasal discharge
- Persistent nasal drainage and congestion
- Upper tooth pain
- Frontal headaches and/or facial pressure
- Fever, fatigue and malaise
Treatments for Tympanic Membrane Perforation
When tympanic membrane perforations occur in both children and adults, they are initially observed for several months to allow the holes to spontaneously heal. If drainage occurs, it can temporarily be treated with antibiotic ear drops and by keeping the ear dry. If the perforation is persistent or chronically drains, a tympanoplasty is usually necessary. In children this is usually performed between ages 5-8 to allow the age at which ear infections occur to pass which could lead to failure of the graft and operation. The operation is almost always performed as an outpatient surgical procedure and requires the ear to remain dry for several weeks afterwards. The hearing is temporarily diminished as the eardrum is allowed to heal. The biggest drawback of tympanoplasty is that the tissue graft does not survive in 7-10% of cases and a revision surgery may be necessary.
BOTOX® Cosmetic
Treats Fine Lines and Wrinkles
Botox can inhibit lines and wrinkles from forming and becoming etched into the permanent facial appearance. This aging is typically seen around the outer corners of the eyes and on the forehead.
It’s never too late to prevent wrinkles from forming. Men and women of all ages and ethnicities are having tremendous results with BOTOX® treatments. Lines and wrinkles that appear around the eyes (“crows feet”) and forehead are an inevitable part of normal aging. These furrows are caused by skin that has lost its elasticity due to repeated contractions of the muscles responsible for facial expression. Prior to BOTOX®, surgery was the only option available for restoring a more youthful look to these facial regions. Botox has revolutionized the treatment of aging to the upper one third of the face and is one of today’s most popular non-surgical procedures for men and women.
One ten minute treatment and a few tiny injections gets results in just days.
What is Botox® Cosmetic?
BOTOX® is a non-surgical, physician administered product used to temporarily improve (smooth out) facial lines and wrinkles that typically occur in the forehead and around the eyes. It is safe, simple, and FDA approved for use in men and women older than age 18. BOTOX® is a synthetic and purified form of a protein originally made from the Clostridium Botulinum bacteria. This protein works by inhibiting the release of molecules from nerve fibers which enable muscle contraction. When injected into the muscles that cause facial animation, these muscles relax (usually within 3-4 days) and allow the related lines and wrinkles to “smooth out.” BOTOX® can also be used to prevent the initial formation of fine lines and wrinkles in the forehead and around the eyes. Botox typically lasts for 3 months before the muscles regain function and the fine lines recur. As repeated treatments occur, however, the effect of the treatment typically gets longer and may approach 6 months.
Common Signs of Facial Aging
- Forehead lines & wrinkles
- Thinning of the lips
- Fine lines around the mouth
- Crow’s feet located at the corners of the eyes
- Deep furrows in the cheek (Nasolabial Folds)
- Frown lines below the mouth (Marionette Lines)
- Chin creases and jawline indentions
- Tear troughs under the lower eyelids
- Blocks muscle contractions and PREVENTS fine line & wrinkle FORMATION
- Inhibits muscle motion to SMOOTH OUT EXISTING fine lines & wrinkles
- Botox restores a refreshed, youthful facial appearance around the eyes and forehead
- Achieves results in a few days which lasts for 3-4 months
- Botox is an office treatment with no downtime
- Botox has an extraordinary long safety record and has virtually no complication risk when performed in experienced hands
Expert Injector
Administering injectable treatments requires great skill and a comprehensive knowledge of the facial anatomy of each ethnic group. No two individuals are alike – each face requires an individualized treatment plan, dosage, and injection technique. Dr. Gunnlaugsson is an experienced injector who has performed Botox® on thousands of patients.
Trust a Fellowship Trained Facial Plastic Surgeon
Dr. Gunnlaugsson is a fellowship-trained facial plastic surgeon and is certified by the American Board of Otolaryngology – Head and Neck Surgery (ABOHNS). He was board certified by the American Board of Facial Plastic and Reconstructive Surgery (ABFPRS) from 2004 to 2017. This dual Board certification involved meeting and exceeding rigorous board standards by passing exams and completing additional specialized training/education in cosmetic surgery of the head and neck. Dr. Gunnlaugsson was awarded the Jack Andersen Memorial Award for obtaining the highest oral and written score on his Facial Plastic Surgery Board Examination. Fellowship training also afforded Dr. Gunnlaugsson the privilege of additional learning under the tutelage of other renowned surgeons. From this he developed the added skills and techniques that his patients benefit from today.
Juvederm® and Juvederm XC®
Treats Fine Lines and Wrinkles
Lines & wrinkles are part of the aging process. Juvederm is part of the anti-aging solution.
Collagen loss is a main cause for fine lines and wrinkles that appear on the face and body. These changes are part of the normal aging process and are exacerbated by environmental damage (sunlight and tobacco use). These fine lines are most noticeable in the upper and lower lips. Collagen is the support system under the skin, located in the dermis, that keeps the skin firm and youthful looking. In addition, soft tissue volume loss occurs as we age and worsens the appearance of these fine lines. Injectable volume restoration with Juvederm plumps up the lines and wrinkles immediately and can dramatically decrease the visual signs of aging.
What is Juvederm®?
Juvederm® is a cosmetic “filler” (injection treatment) made from hyaluronic acid, a naturally occurring substance in the human body. It attracts and binds to water to keep the skin hydrated, firm, and contoured. Juvederm® replaces the collage that is depleted as we age and therefore corrects the volume loss that allows fine lines and wrinkles to form. Juvederm® can restore a youthful balance to the nasolabial folds around the cheek. Juvederm is especially effective in restoring volume to the lips, which thin and elongate as we age. Hyaluronic acid injections offer significant results lasting 12 months or longer, especially if maintained every six to twelve months.
Common Signs of Facial Aging
- Forehead lines & wrinkles
- Thinning of the lips
- Fine lines around the mouth
- Crow’s feet located at the corners of the eyes
- Deep furrows in the cheek (Nasolabial Folds)
- Frown lines below the mouth (Marionette Lines)
- Chin creases and jawline indentions
- Tear troughs under the lower eyelids
- Juvederm is a smooth gel made of naturally occurring hyaluronic acid – it absorbs water like a sponge to add volume and hydration to the skin
- Juvederm is FDA approved and has a long safety record
- Juvederm is exceptional for restoring youthful qualities to fine lines and the lips
- Deeper folds can also be corrected and contoured
- Juvederm XC with Lidocaine provides comfort immediately
- Painless injections are done “in office” under local anesthesia with no significant recovery time – the results are immediate
Radiesse®
Treats Fine Lines and Deeper Wrinkles
Welcome back your own natural appearance & smooth out the signs of aging. Radiesse results are natural…immediate…long lasting.
Each one of us ages at a different rate caused by various factors. The main elements that cause facial aging involve changes in the bones along with the loss of fat, collagen, and elastin from the facial tissues. This loss of facial volume, along with skin texture changes, leads to alterations in our appearance as we grow older. Early prevention, by starting non-invasive injectable volume restoration, can delay the need for more aggressive anti-aging measures and are key in lessening the visual signs of aging.
What is Radiesse®?
Radiesse® is a cosmetic “filler” (injection treatment) that provides immediate volume to smooth out the early signs of aging. Composed of smooth microspheres of calcium hydroxyapatite (found naturally in the body), it acts as soft tissue filler while it works with your body to stimulate collagen growth. This can allow the regeneration of new connective tissue and provide extended correction to areas of the facial skeleton where volume loss has occurred. Because of its density, Radiesse is ideal for the nasolabial folds and smile lines in the cheeks along with other areas of soft tissue loss. It is also used by Dr. Gunnlaugsson to restore a youthful quality to the lower eyelid and avoid surgical procedures such as Blepharoplasty. Results are natural looking, immediate, and long lasting (often 1.5-3 years).
Common Signs of Facial Aging
- Forehead lines & wrinkles
- Thinning of the lips
- Fine lines around the mouth
- Crow’s feet located at the corners of the eyes
- Deep furrows in the cheek (Nasolabial Folds)
- Frown lines below the mouth (Marionette Lines)
- Chin creases and jawline indentions
- Tear troughs under the lower eyelids
- Radiesse is FDA approved and has a long safety record
- Radiesse is ideal for areas of soft tissue volume loss
- Radiesse easily fills in facial depressions and folds
- Painless injections are done “in office” under local anesthesia with no significant recovery time – the results are immediate
- Radiesse promotes the formation of new collagen and stimulates long lasting facial volume restoration
- Radiesse has been used in cosmetic and reconstructive treatments in hundreds of thousands of patients
- Celebrities start early with less invasive procedures …. to reverse and maintain a youthful appearance
Expert Injector
Administering injectable treatments requires great skill and a comprehensive knowledge of the facial anatomy of each ethnic group. No two individuals are alike – each face requires an individualized treatment plan, dosage, and injection technique. Dr. Gunnlaugsson is an experienced injector who has performed Botox® on thousands of patients.
Trust a Fellowship Trained Facial Plastic Surgeon
Dr. Gunnlaugsson is a fellowship-trained facial plastic surgeon and is certified by the American Board of Otolaryngology – Head and Neck Surgery (ABOHNS). He was board certified by the American Board of Facial Plastic and Reconstructive Surgery (ABFPRS) from 2004 to 2017. This dual Board certification involved meeting and exceeding rigorous board standards by passing exams and completing additional specialized training/education in cosmetic surgery of the head and neck. Dr. Gunnlaugsson was awarded the Jack Andersen Memorial Award for obtaining the highest oral and written score on his Facial Plastic Surgery Board Examination. Fellowship training also afforded Dr. Gunnlaugsson the privilege of additional learning under the tutelage of other renowned surgeons. From this he developed the added skills and techniques that his patients benefit from today.
We look forward to caring for you!
(803) 509-7200